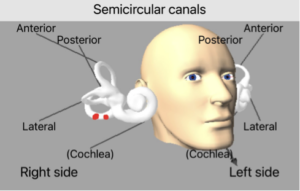
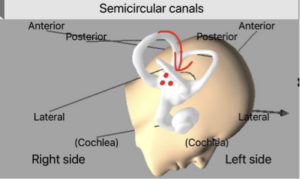
The most common vestibular disorder is the condition of Benign Paroxysmal Positional Vertigo (BPPV), which accounts for up to 40% of all patients experiencing vertigo. This condition is the result of otoconia (inner ear crystals) migrating into one of the semicircular canals (head turn sensors) of the inner ear. The majority of cases can be readily treated with canalith repositioning procedures, with the most frequently utilized being the Epley maneuver. These repositioning procedures aim to move the crystals from the semicircular canal via a series of timed head movements. Canalith repositioning is quite effective at resolving symptoms in an expedient manner.
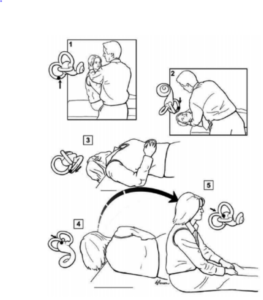
Epley maneuver steps shown
The Epley maneuver is designed to treat the most common variant, posterior canal BPPV. This maneuver requires the patient to turn their head 45 degrees toward the affected side while seated on a bed or exam table (position 1). The patient is then reclined backward into a supine position with their head turned 45 degrees toward the affected ear and with their head tilted backward (position 2). After a period of around 30 seconds the head is then turned away from the affected ear toward the opposite shoulder with the head still tilted backward (position 3). The patient then rolls onto their side, away from the affected ear, with their nose pointed downward toward the floor (position 4). The patient is then brought upright to a seated position (position 5).
Despite the effectiveness of the Epley maneuver, some positions may be difficult for some patients to maintain. We first described a case report of a modification that we made to the Epley maneuver for a patient with recent arthroscopic rotator cuff repair in 2021. This patient had right posterior canal BPPV and was unable to complete position 4 of the Epley maneuver due to recent shoulder surgery. This modification to the Epley maneuver was successful in resolving the patient’s symptoms with one treatment and has been successful in alleviating several other patients’ symptoms since that time. It is worth noting that this patient also attempted another maneuver that didn’t require them to roll onto their side, the Half Somersault, both in office and at home without any change in symptoms.
Our Modification to the Epley Maneuver for BPPV
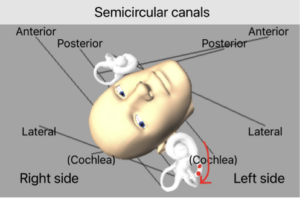
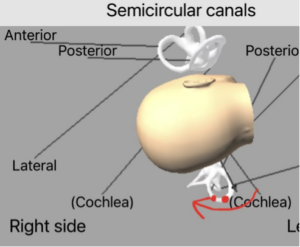
The modification involves completing position 1,2 and 3 of the Epley maneuver as described above. In position 2 we keep the patients head nearly upside down with the head turned 45 degrees toward the affected side. In position 3 we turn the patients head toward the opposite side, once again with their head extended backward to the point that it is nearly upside down. Instead of going in to position 4, rolling the patient on their left side, we quickly sit the patient upright and have them point their nose downward, looking down toward their lap. We essentially made position five include an extreme head tilt forward and skipped position 4 altogether.
Below is a demonstration of the modification for the right ear with the otoconia movements in red:
Update on Modification
Since we first described this in 2021 we have completed this maneuver on a total of 15 patients. This modification was utilized in cases that precluded the patient from being able to roll onto their side to complete a standard Epley maneuver.
Some instances where we have used this include patients with a colostomy bag, recent knee surgery, recent shoulder surgery, and for larger individuals that were unable to roll over onto their side in our exam chair, even with assistance.
This modification resulted in complete symptom resolution in 73% (11 out of 15) of the patients after only one maneuver. A total of 20% (3 out of 15) patient’s symptoms were not resolved. All 3 of these individuals were unable to roll over in our exam chair but were capable of doing so safely on a larger surface, such as their bed. These 3 individuals were all able to successfully complete home Epley maneuvers, completed the traditional way, with symptom resolution. The modified Epley was felt to be ineffective for these 3 patients due to their inability to obtain the appropriate head positions for this modification.
Of these individuals that it was found to be ineffective for, we noted that 1 of the patients could not extend their head backward, which likely impeded the otoconia from migrating around the bend in the posterior canal. The other 2 individuals were unable to quickly sit upright and then tilt their head forward, which is the point in this maneuver in which the otoconia should be exiting the canal and entering the vestibule. Lastly, 7% (1 out of 15) did not show resolution with the modified Epley in office or with home Epley maneuvers completed in the traditional manner. This individual’s symptoms gradually resolved over the period of a few months.
This is a relatively small sample size and we need more data on this maneuver to better understand just how useful this modification is. At this time though, there is at least proof of concept that this can effectively resolve posterior canal BPPV in some patients.
We are not advocating completing this modification rather than a traditional Epley maneuver for the majority of patients, but rather we pose this as a reasonable modification that can be made for some patients that may be unable to complete a traditional Epley maneuver.







