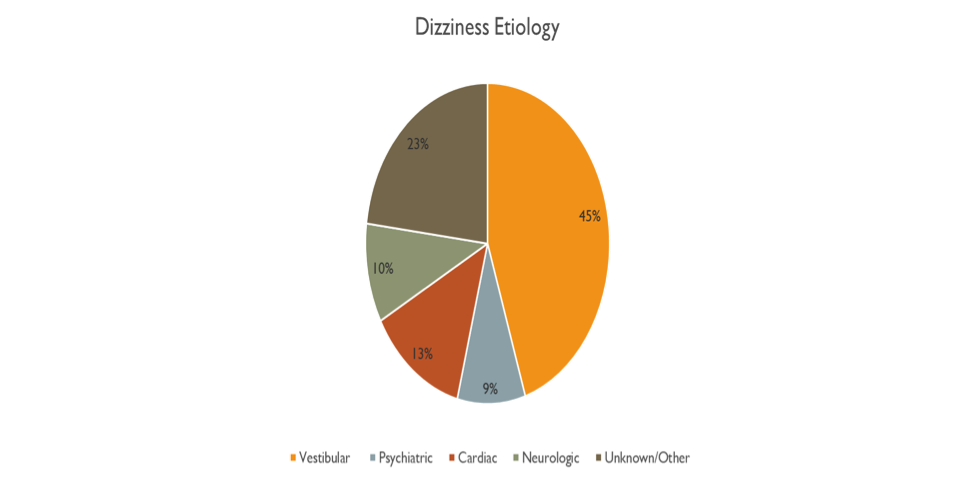
Vestibular disorders are the most common reason for symptoms of dizziness regardless of the clinical setting. A five study average reveals that vestibular disorders account for around 45% of all dizziness and are much more common than cardiovascular or potentially life threatening neurologic causes for dizziness. Despite the magnitude of individuals suffering from vestibular type dizziness, these disorders are historically poorly managed and frequently misdiagnosed.
Recent studies have shown up to an 80% misdiagnosis rate for those suffering from vestibular disorders in an Emergency Department setting.
Vestibular disorders, while not directly life threatening, can lead to reduced quality of life, reduced productivity, higher fall risk, and higher rates of anxiety and depression. Vestibular assessment typically falls within the specialty area of otolaryngology. Even within this specialty area, there is no commonly agreed upon criteria for what comprises a vestibular assessment, likely further contributing to misdiagnosis.
- Prevalence and characteristics of diagnostic groups amongst 1034 patients seen in ENT practices for dizziness
- Spectrum of dizziness visits to US emergency departments: cross-sectional analysis from a nationally representative sample
- Vertigo and dizziness in the emergency room
- Diagnosing and treating dizziness
- Etiologic distribution of dizziness and vertigo in a referral-based dizziness clinic in South Korea
Videonystagmography (VNG)
The most commonly performed vestibular testing protocol is the VNG, which typically consists of monitoring for spontaneous or gaze evoked nystagmus, measuring ocular motor function, assessing for positional nystagmus and caloric irrigations. We have previously discussed the limitations of the VNG here.
The only component of this exam that measures vestibular ocular reflex (VOR) function, which is the primary function of the human vestibular system, is the caloric irrigation. Caloric testing assesses the horizontal semicircular canal and VOR at .003Hz. This is an extremely low frequency (slow head speed) at which it is nearly impossible to move your head. The natural human VOR works across a wide range of frequencies (.05 Hz to 5 Hz) and it is key to note that someone can have an isolated deficit at just one frequency (head speed range). As such, deficits can be missed if multiple frequencies are not assessed.
Additional measures such as vHIT, vibration, VEMP, and rotary chair testing are all complimentary measures to the traditional VNG which can increase the diagnostic utility of the assessment; however, currently there are few locations that complete a truly comprehensive vestibular work up. This limited access is likely at least partially related to reduction in reimbursement, high equipment cost, and a limited supply of trained professionals.
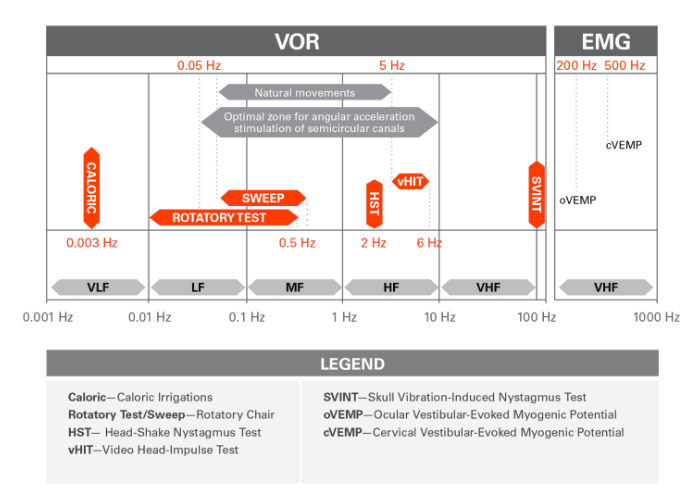
Image courtesy Dumas et al 2017
Limitations of VNG
BPPV is by far the most common vestibular condition and it is often easily treated with canalith repositioning procedures such as the Epley maneuver. BPPV has a high negative exam rate and if the examiner is not aware of this, then the diagnosis could be missed. Meniere’s disease may present with normal VNG results, especially in the early stages of the disease process. A vestibular schwannoma that is small or limited to the inferior branch of the vestibular nerve might be missed by VNG. Third mobile window syndromes are likely to be missed by a VNG.
Somewhat anecdotally, I have seen multiple cases of high frequency VOR (vHIT) abnormalities with normal caloric function. I have observed this phenomenon in several elderly patients and it is unclear if this could be an age related decline to the system. The VNG also has the potential to miss deficits, even with conditions such as vestibular neuritis which can cause permanent damage to the peripheral vestibular end organs with only one episode.
It is clear that the VNG has the potential to miss some vestibular disorders and this is only exacerbated if the examiner training is limited.
A Closer Look at Vestibular Neuritis
The conditions of vestibular neuritis/labyrinthitis are thought to be a viral insult to the inner ear structures in most instances and they have the potential to permanently damage any of the peripheral vestibular end organs. Since these two conditions are so similar, with the only difference being the portions of the ear are impacted, I will refer to both of these conditions as VN for brevity.
VN is a common cause for dizziness symptoms and its impacts to the vestibular system are amongst the best studied. In most instances VN impacts multiple end organs, with isolated deficits to only one end organ being the minority of cases.
Vestibular neuritis/labyrinthitis and nerve branch impacted (5 study average)
| Superior Branch Only | Superior and Inferior Branch | Inferior Branch Only |
| 46% | 46% | 4% |
- Vestibular neuritis: Involvement and long-term recovery of individual semicircular canals
- Vestibular neurolabyrinthitis: a follow-up study with cervical and ocular vestibular evoked myogenic potentials and the video head impulse test
- Lesion Patterns and Possible Implications for Recovery in Acute Unilateral Vestibulopathy
- The spectrum of acute vestibular neuropathy through modern vestibular testing: A descriptive analysis
- Vestibular neuritis affects both superior and inferior vestibular nerves
Vestibular neuritis/labyrinthitis and end organ affected (3 study average)
| Horizontal SCC | Superior SCC | Utricle | Saccule | Posterior SCC |
| 95% | 81% | 69% | 35% | 35% |
- Lesion Patterns and Possible Implications for Recovery in Acute Unilateral Vestibulopathy
- The spectrum of acute vestibular neuropathy through modern vestibular testing: A descriptive analysis
- Vestibular neuritis affects both superior and inferior vestibular nerves
In most cases of VN, the horizontal semicircular canal is impacted. This aids in the ability to measure the degree of deficit, as this is the most readily assessed vestibular end organ.
Using an average of the same data sets above, VNG would detect around 92% of cases of VN. Another way of saying that is only 8% of VN impacts the vestibular system to a measurable degree that is not detectable by a caloric irrigation. This 8% would only be detected by adding vHIT and VEMP testing to the test protocol. The VNG actually does a pretty good job at detecting most cases of VN.
Steps toward improvement
One step toward improving the management of patients with vestibular disorders is to increase the availability of uniform comprehensive vestibular assessment. There are multiple reasons for this current lack of availability. While not an easy task, greater access would result in better identification of patients with vestibular disorders.
Another step would be better education for specialists working with these conditions. Many otolaryngology and audiology programs provide only limited training, both at the clinical and classroom levels. More training in these programs would likely lead to more efficient diagnosis and better outcomes for those dealing with vestibular disorders. Further training with the emergency department and internal/family medicine would also likely improve outcomes, as these are the frontline professionals evaluating dizzy patients.
Knowledge of the vestibular system and vestibular assessment is important even for those who cannot or do not perform comprehensive vestibular evaluations. It is important to know when referral for additional work up is indicated. Lastly, if all you have access to is VNG equipment, then is important to know the limitations and when to refer for additional testing.







